June 2015 Case of the Month
62 year-old male with longstanding history of acid reflux presented to the ER with abdominal discomfort and melena. CT of the abdomen showed a possible mass in the stomach body. Upper endoscopy revealed a single large ulcer in the body. Multiple biopsies were taken of the ulcerated area. What is your diagnosis?

Expansion of gastric lamina propria by lymphoid infiltrate.
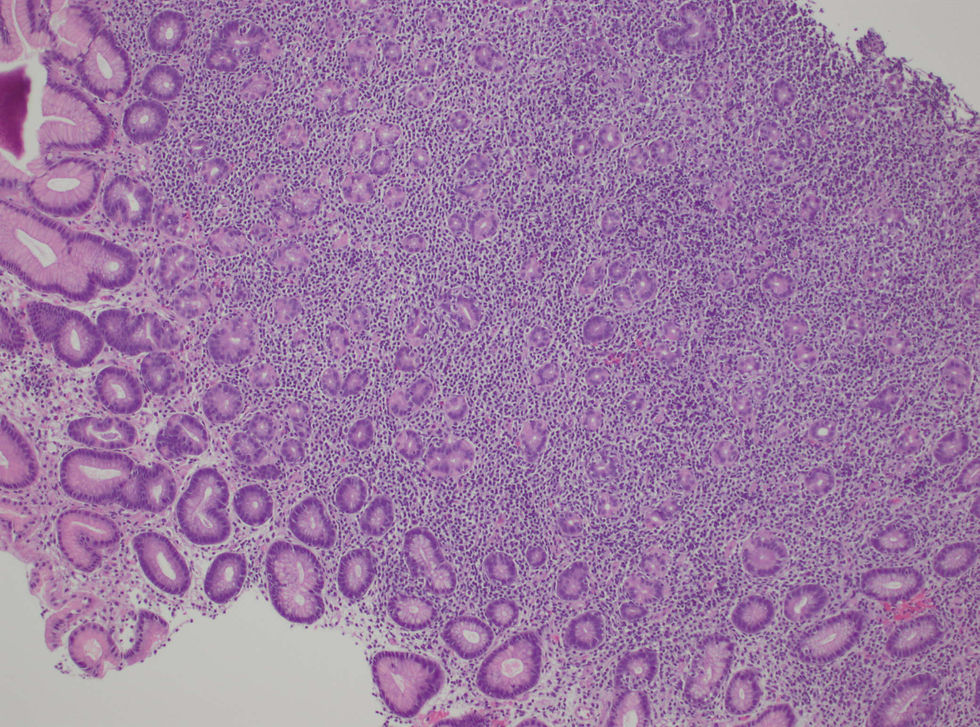
Distortion of gastric pits by lymphoid infiltrate.

Mostly negative, indicating a skewed kappa:lambda ratio or clonal plasma cell component.

Expansion of gastric lamina propria by lymphoid infiltrate.
Scroll Down for Answer
June 2015 Case of the Month
Answer: Extranodal Marginal Zone Lymphoma of Mucosa-Associated Lymphoid Tissue (MALT Lymphoma)
The gastric biopsy shows marked expansion of the lamina propria by a monomorphous lymphoid infiltrate. Scattered lymphoepithelial lesions and destruction of the gastric pits is noted. By immunohistochemistry, the infiltrate is CD20(+), CD3(-), CD5(-), CD10(-), Bcl6(-), Bcl2(+), CD43(-), and cyclin D1(-). In addition, a CD138 stain highlights collections of plasma cells which show kappa light-chain restriction by immunohistochemistry. These features are thus consistent with a MALT lymphoma of the stomach. An H. pylori immunostain was negative in this case, though infection by this organism has a strong association with gastric MALT lymphoma. Some studies have shown a lower incidence as well as detection rate of H. pylori as lymphoma evolves from gastritis. Roughly 6-26% of gastric MALT lymphomas may show a t(11;18) translocation of the BIRC3 (formerly API2 gene) and MALT1 genes; however, chromosomal analysis or FISH testing were not performed in this case. In general, MALT lymphomas behave in a biologically indolent manner.

